Payor
PAYOR
A Payor is defined as the party that will be responsible for paying for the services tracked in the system. A Payor can be an insurance company, an organization (through a service contract with that organization), or when the client themselves, which is defined as "Self-Payor". The Self Payor is the only one that is pre-loaded into a new system. In order to obtain accurate billing reports, you'll need to load all Payors to which your organization bills. Until this information has been loaded into the system, this field will appear blank. Payors can either be loaded all at one time, or can be loaded as needed as part of entering new client information. Each Payor can have multiple "plans" which in turn are linked to a fee schedule.
ADDING A PAYOR
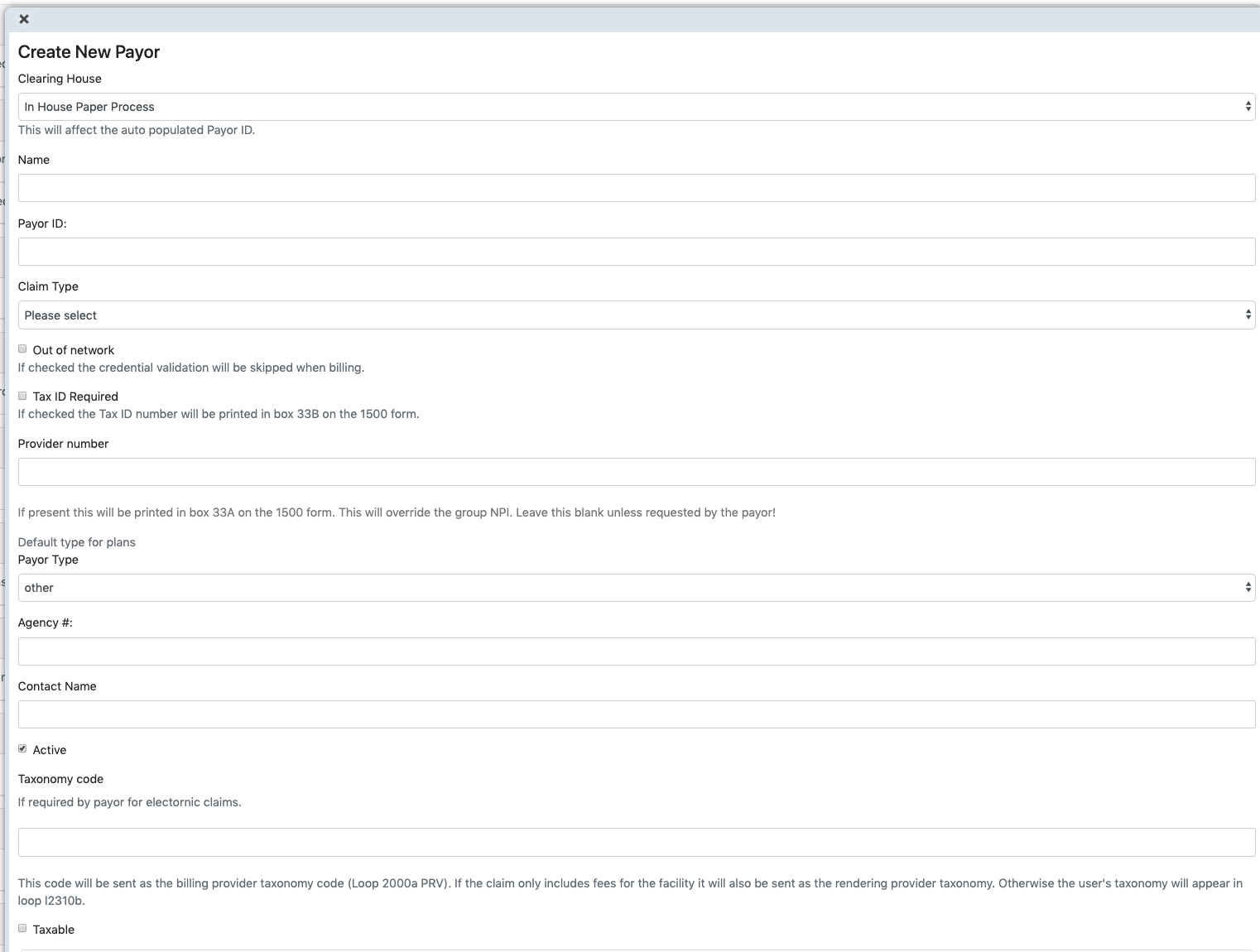
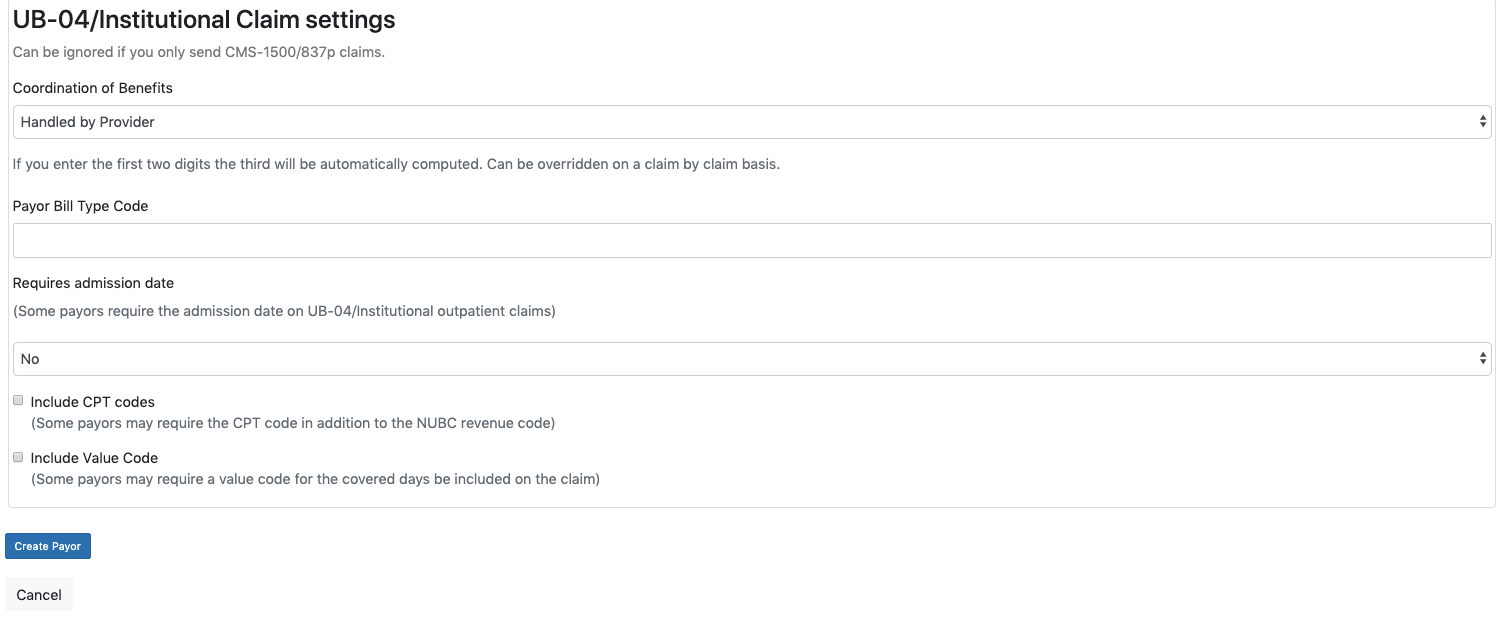
- To add a new payor to EMR-Bear, Go to dashboard -> Billing on the top menu bar.
- Hovering over the Billing menu will generate a dropdown menu with payor option in it.
- Or you can also go to Dashboard and in the Billing subsection click on Payor.
- Clicking payors will take you to the page where you can add a new payor.
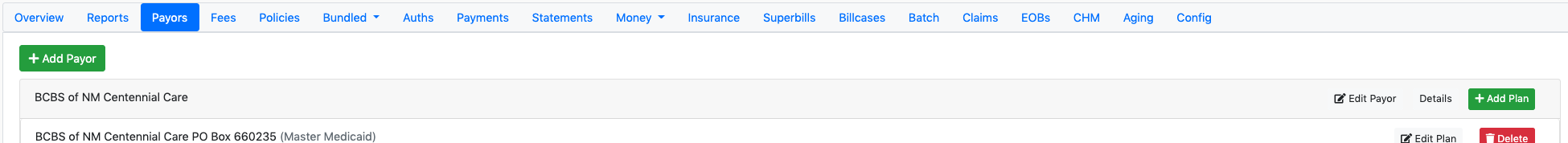
- This is a list of payors. Under each payor is a list of 1 or more plans. Click on Add new payor to add a new payor to the system.
PAYOR PLAN
The definition of 'Plan' in EMR-Bear is a specific "benefit plan" offered by the Payor that a given client might be associated with. Most Payors offer several benefit plans, and each of them might have a different set of benefits for different clients enrolled in that plan (i.e., some plans may cover certain procedures, others might not, or reimbursements may differ from plan to plan).
Many times the billing address that receives claims for a given plan is different from that of another plan for the same Payor. For these reasons, one Payor may have several plans associated with them. EMR-Bear provides a transparent way to associate your client's insurance companies to the correct Payor and (benefit) Plan under that Payor.
- Once you have a payor, you can add a plan for the payor. A payor can have multiple plans.
- Click on Add Plan to add a payor plan.
- NOTE: You will need to back date the plan and expire any old plans or you will receive errors when attempting to bill.
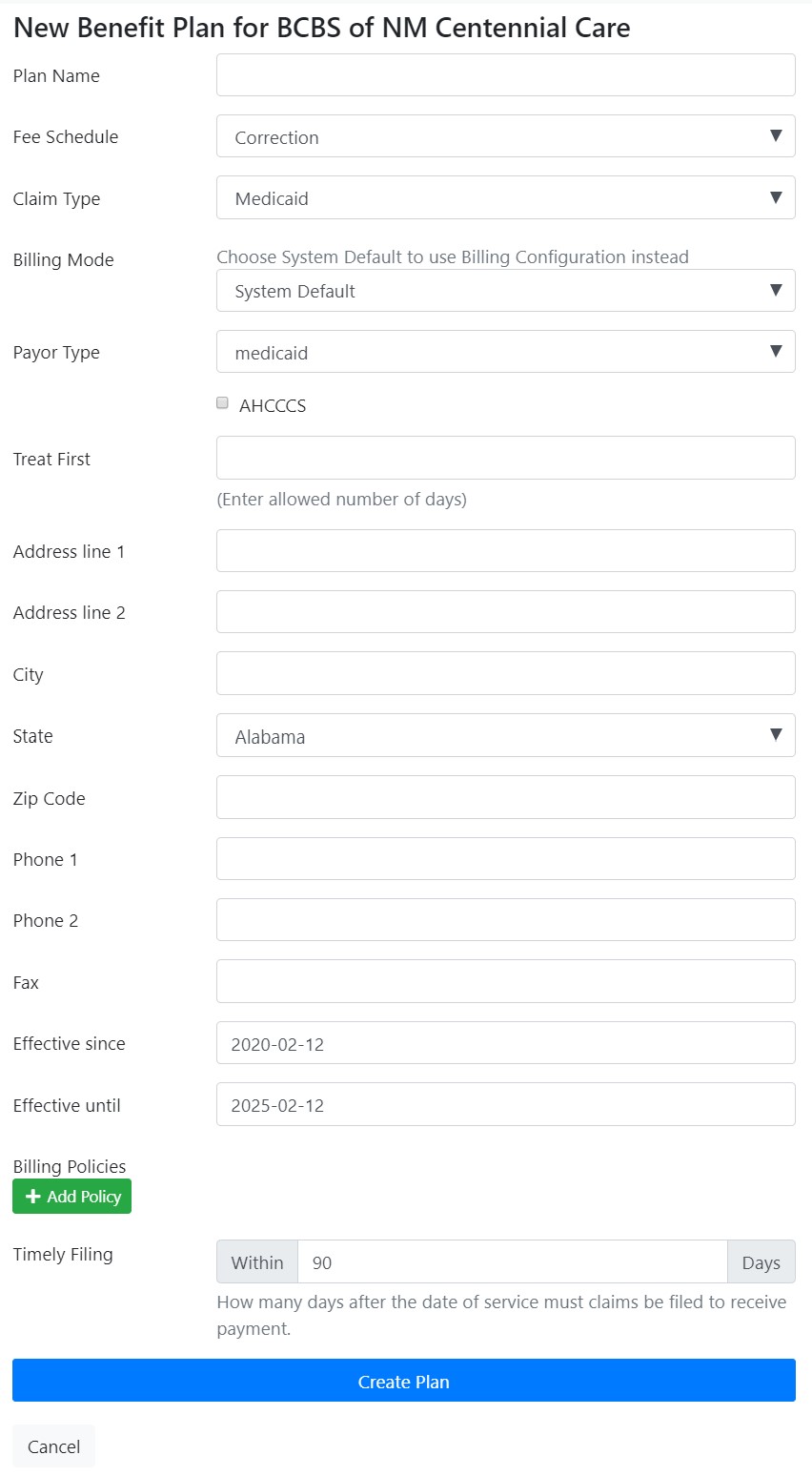
- Plan name: the name for this plan (required)
- Fee Schedule: the Fee Schedule associated with this plan. (add link to fee schedule)
- Effective since and Effective until will be pre-populated, however, if these plans reflect a specific contract term, you can use these fields to keep track of the contract's end date.
- Billing policies: allows you to restrict which diagnosis is allowed for which procedure code. There will list of procedures for diagnosis. The billing policies enable extra set of rules for billing. They need to be defined here and assigned to the specific Payor Plan. Whenever a superbill is created using such plan, if a current billing policy is linked to that plan, then the system will run its validation and approve or not the superbill based on those rules. Each Billing Policy can have several Policy Sets. Policy Sets have a collection of procedures and a collection of diagnosis codes. If a procedure on a superbill matches one set, then the set rules will be applied. A plan can take one or more Billing Policies, and each billing policy can have more than one policy set. A billing policy will pass the validation if all matching policy sets pass. A policy will only validate a set for which there's a matching diagnosis. The "Policy Procedures" is a different repository than that of your fees. It is an abstraction that has one single entry per each combination of procedure code and modifiers, regardless of the fee schedule. Meaning that if you have the same procedure code several times in different fee schedules, you only will have it once in the policy procedures repository. The system offers a feature to mass process and create policy procedures from your fee schedules.
Table of Contents
Other Billing Articles
- Fee Schedules
- Fees
- Payor Plan
- Incident to Billing
- User credential for Billing
- User Roles
- Front Desk Billing Configuration
- Certification or Licensure number
- Provider number
- Adding location
- Billcase
- Superbills
- Billing configuration
- Billing the secondary and the tertiary insurance
- Printing claims
- Batch processing printable claims
- EOBs
- Posting Manual EOBs
- Specifying billing codes In the form
- Printing individual claims
- Claims
- Refund / Recoups payment
- Bundled service
- Taxes
- Aging report
- Payments
- Creating Statements/Copay Report
- Fixing a denied claim
- UB-04
- Claim printing settings

